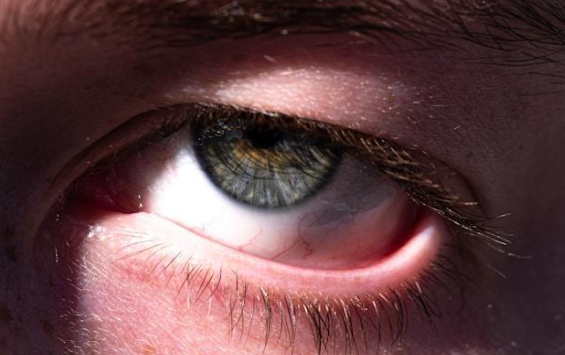
Recognizing and Treating Summer Conjunctivitis (Pink Eye)
Recognizing and Treating Summer Conjunctivitis (Pink Eye)
Summer brings sunshine, vacations, and poolside fun, but the season also increases the risk of conjunctivitis. As temperatures rise, so does exposure to irritants like chlorine, pollen, dust, and bacteria, all of which can inflame the thin tissue that lines your eyes.
Here’s an overview to help you understand how to recognize, treat, and prevent summer conjunctivitis.
What Is Summer Conjunctivitis?
Conjunctivitis is the inflammation or infection of the conjunctiva, the clear membrane that covers the white part of your eye and the inside of your eyelids. When this thin tissue becomes irritated or infected, the eye turns red or pink, giving the condition its nickname: pink eye.
While conjunctivitis can strike at any time, summer introduces a unique set of triggers. This season, people are more likely to swim in pools, visit crowded places, and spend time outdoors, all of which can increase the risk of
infection or irritation.
Types of Conjunctivitis
Conjunctivitis comes in various forms, and some are highly contagious. During the summer, you typically see an increase in three primary types:
Viral Conjunctivitis
This is typically caused by adenoviruses, a family of viruses responsible for the common cold and other upper respiratory infections. Its highly contagious nature means it can spread rapidly, especially in environments where people are in close contact. It frequently starts in one eye and then, almost inevitably, spreads to the other within a few days. Accompanying symptoms often include a sore throat, runny nose, or fever.
Bacterial Conjunctivitis
This results from an infection from bacteria, such as Staphylococcus aureus or Streptococcus pneumoniae. This type is also highly contagious and often presents with a more noticeable, thick discharge that can be yellow, green, or white. This discharge can be so substantial that it causes eyelids to stick together, particularly after sleep, making it difficult to open the eyes in the morning. Unwashed hands, contaminated surfaces, or even shared personal items can increase transmission risks.
Allergic Conjunctivitis
Unlike viral or bacterial pink eye, allergic conjunctivitis is not contagious. It’s triggered when your eyes react to allergens like pollen, grass, mold spores, or pet dander, common in the warmer months. If you suffer from seasonal allergies, you’re more prone to this type of conjunctivitis. Rubbing your eyes may feel tempting, but it only worsens the inflammation.
Recognizing the Symptoms
Summer conjunctivitis can look different depending on the cause, but a few hallmark signs are common:
- Red or pink coloration of the whites of the eyes
- Itchy or burning sensation
- Watery or thick discharge (clear in allergies or viral, yellow/green in bacterial)
- Crusty eyelids or lashes in the morning
- Swollen eyelids
- Increased tear production
- A gritty feeling in the eye
- Light sensitivity in more severe cases
If symptoms include pain, vision changes, or intense sensitivity to light, it’s time to contact an ophthalmologist or eye surgeon.
How to Prevent Summer Conjunctivitis
Staying healthy during the summer means taking a few extra steps to protect your eyes. Here are some prevention strategies that can help you avoid conjunctivitis:
- Wear swim goggles in chlorinated pools to protect against eye irritation and bacteria.
- Use allergy medications if you're sensitive to pollen, grass, or dust mites.
- Avoid sharing personal items like towels, eye makeup, or contact lens solutions.
- Keep your hands clean, especially when traveling, after using public transport, or before touching your face.
- Regularly disinfect items like sunglasses, phones, and doorknobs.
- Take care of contact lenses by following proper cleaning and storage procedures. Never use tap water on lenses, and don’t wear them while swimming.
If you have a known allergy or previous bouts of conjunctivitis during the summer, consider seeing an eye specialist before allergy season kicks in to get a head start on treatment.
How Is Conjunctivitis Diagnosed?
A trained eye specialist can typically diagnose conjunctivitis based on symptoms and a basic eye examination. If symptoms don’t improve or are severe, a swab may be taken to identify the specific cause, such as a bacterial or viral infection.
It’s important to note that advanced diagnostic tools ensure accurate evaluation. Quick and proper diagnosis helps guide effective treatment and prevents unnecessary complications.
Treatment Options
The treatment approach for conjunctivitis varies significantly based on its cause. Here are some common approaches taken by eye care specialists:
Viral Conjunctivitis
There is no direct cure for viral conjunctivitis, as it’s caused by a virus, much like the common cold. In most cases, it runs its course within 7 to 10 days. It is recommended to use cool compresses to relieve discomfort in the eye and reduce inflammation. Lubricating eye drops can also help prevent infection from spreading. Specialists generally suggest staying home from work, school, or group activities if your eyes are red and watering.
Bacterial Conjunctivitis
Unlike the viral form, bacterial conjunctivitis can be treated effectively with prescription antibiotic eye drops or ointments. These help reduce the infection’s duration and limit its contagious period. Most people notice improvement within 2 to 3 days of starting antibiotics. You should follow the prescribed dosage and duration, even if the symptoms improve early. You should also avoid wearing contact lenses until the infection clears completely.
Allergic Conjunctivitis
Since this type of conjunctivitis is caused by an allergic reaction, the focus is on reducing exposure to allergens and calming the immune response. Over-the-counter antihistamine eye drops or oral allergy medications are generally prescribed to ease pain and swelling. If you're prone to seasonal allergies, start your allergy medications before peak pollen seasons to reduce your risk.
Chemical or Irritant-Induced Conjunctivitis
This form occurs when the eyes are exposed to irritants like chlorine, smoke, air pollutants, or harsh chemicals. You should immediately flush the eyes with clean water or saline to remove the irritant. Specialists also recommend using soothing lubricating drops to reduce eye irritation. If symptoms persist beyond a few hours or worsen, seek medical attention to rule out
corneal injury or infection.
At
Baptist Eye Surgeons, we’re committed to helping you and your family enjoy a safe, healthy summer. For 40 years, our mission has been to provide the highest standard of eye care to every patient in the Knoxville community. If you have any conjunctivitis concerns or questions, call us at
(865) 413-5433 to
schedule a visit today!